SOWK 486 - Week 09 - Lab Day - Assessments
A presentation at Heritage University in October 2021 by Jacob Campbell and is tagged with Heritage University, BASW Program, SOWK 486w
Description
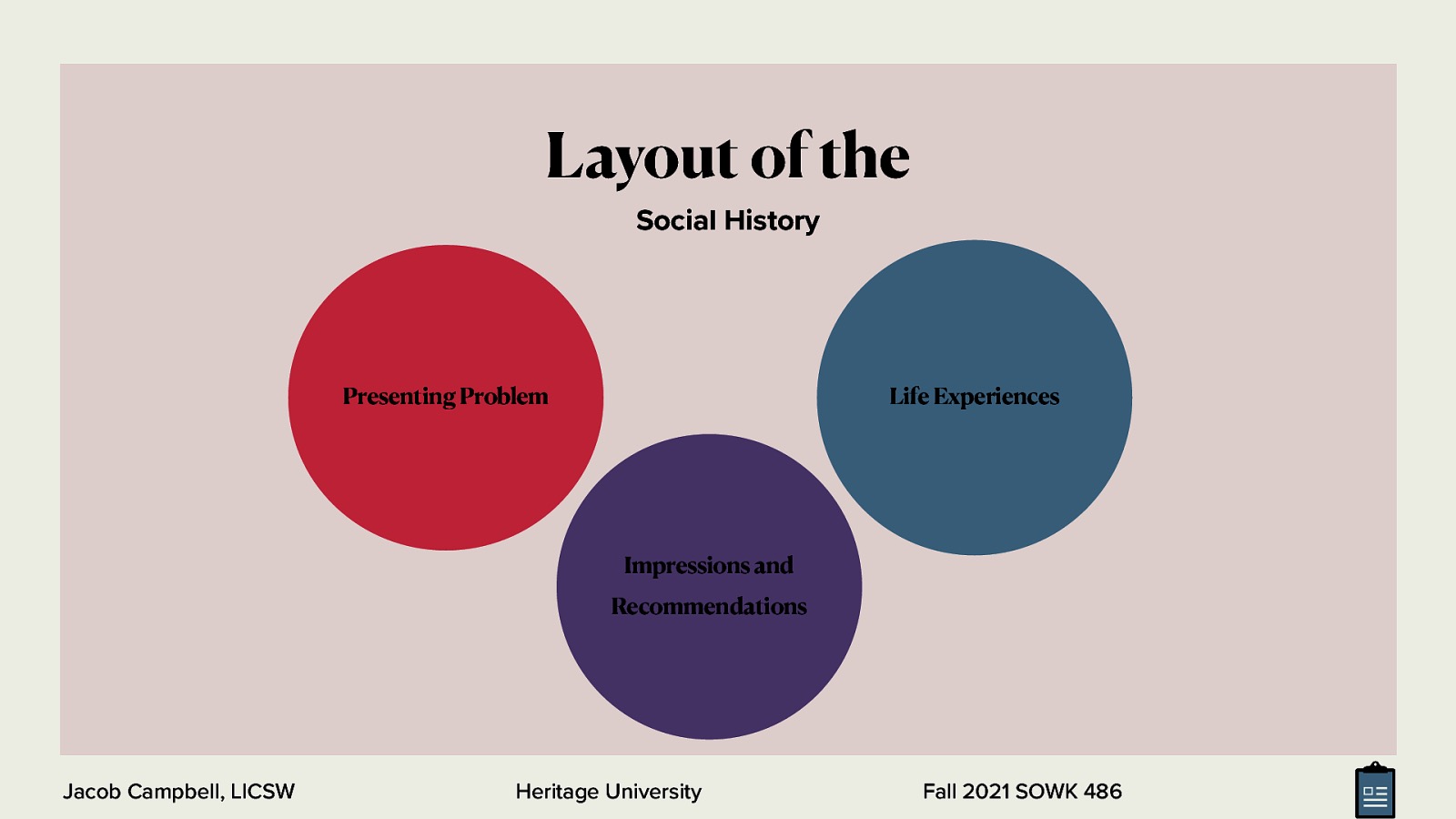
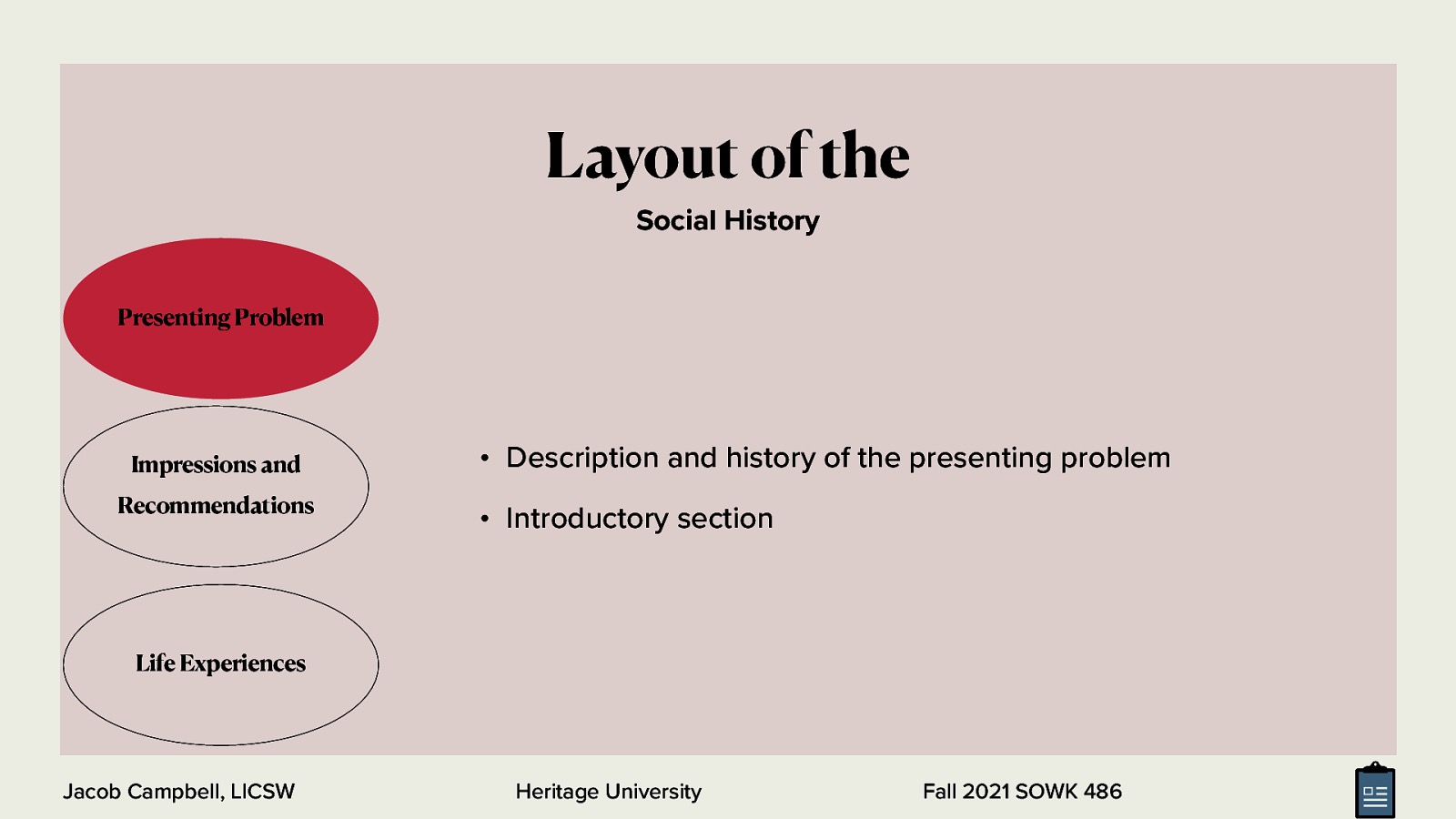
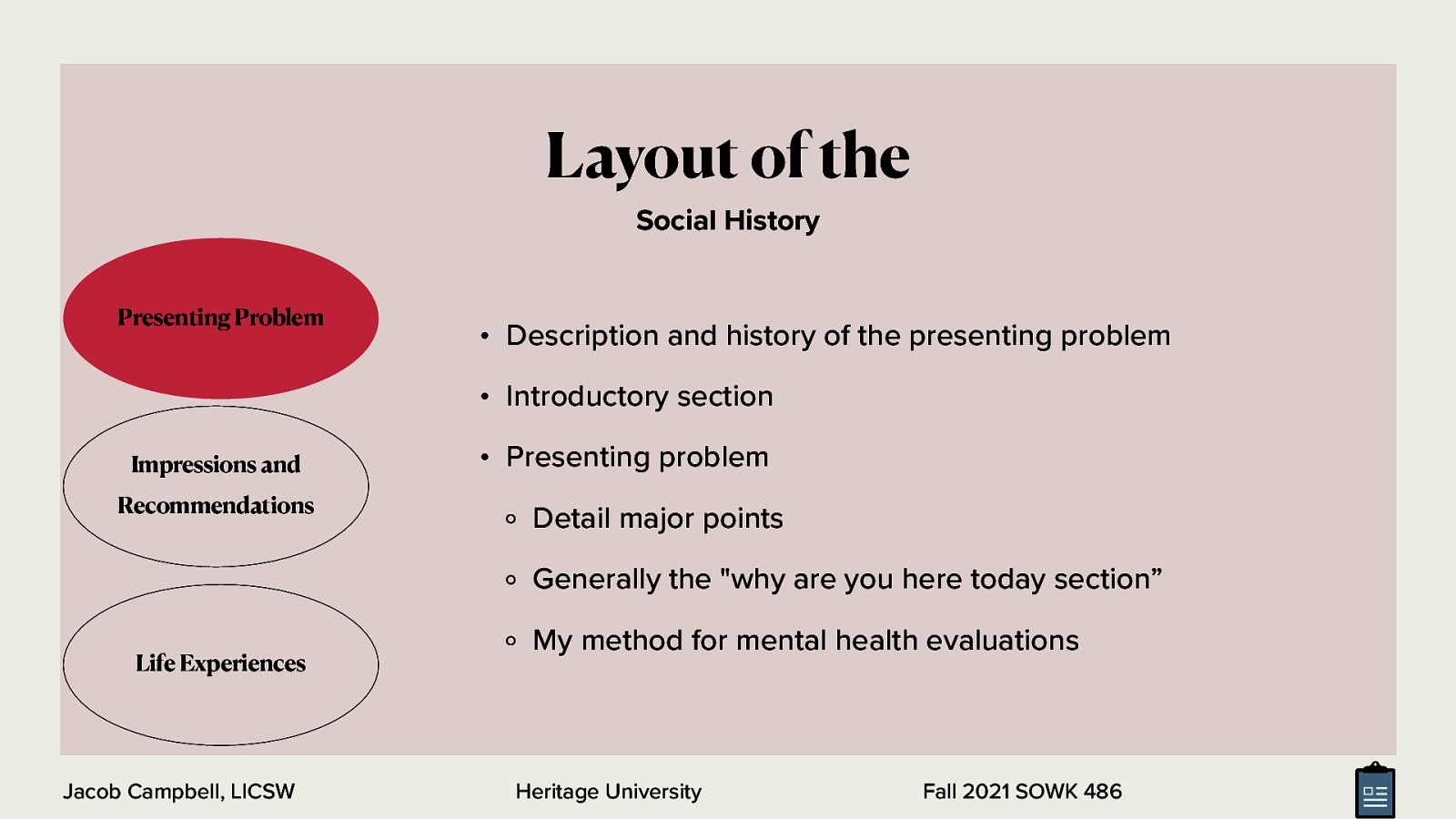
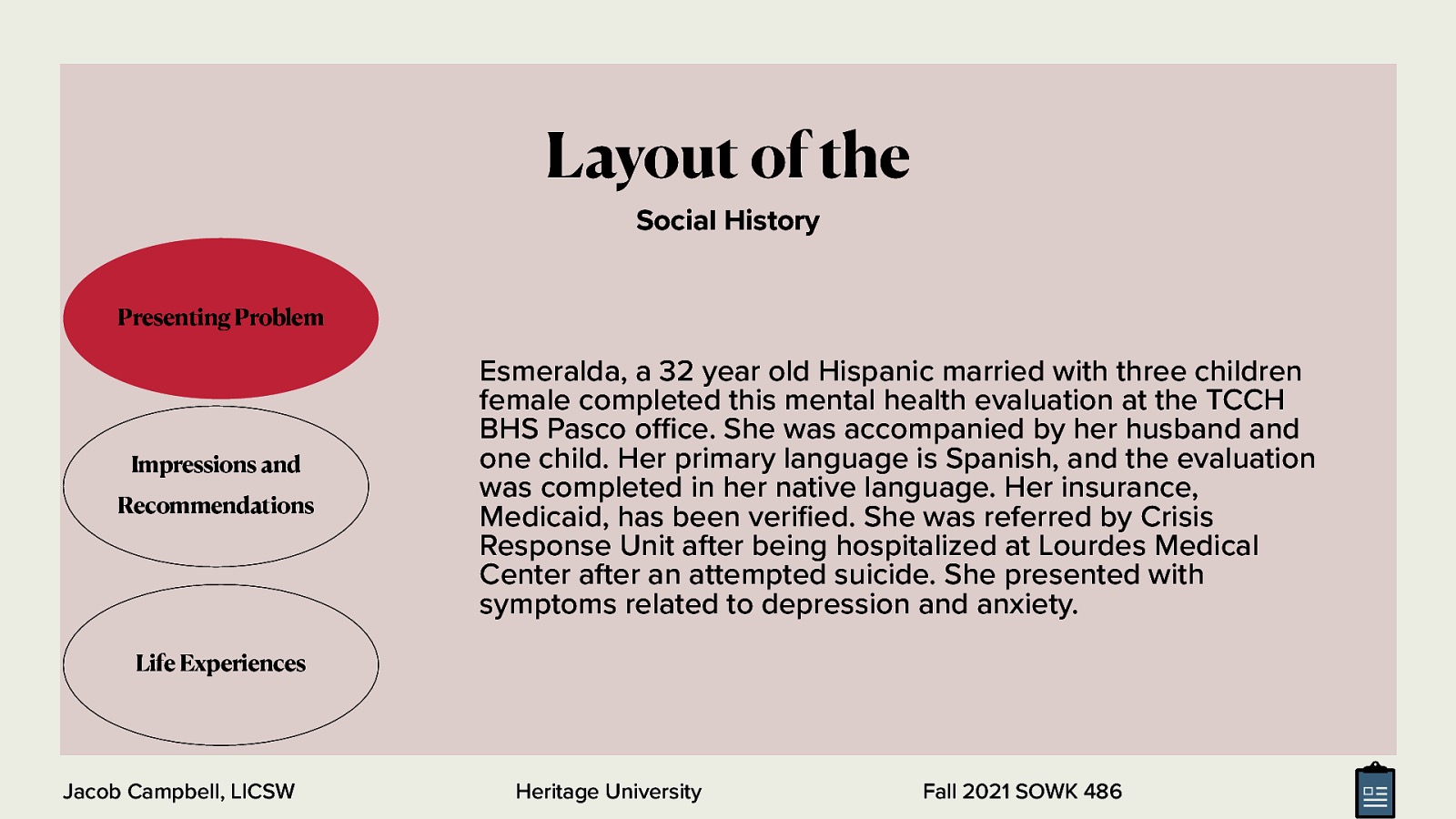
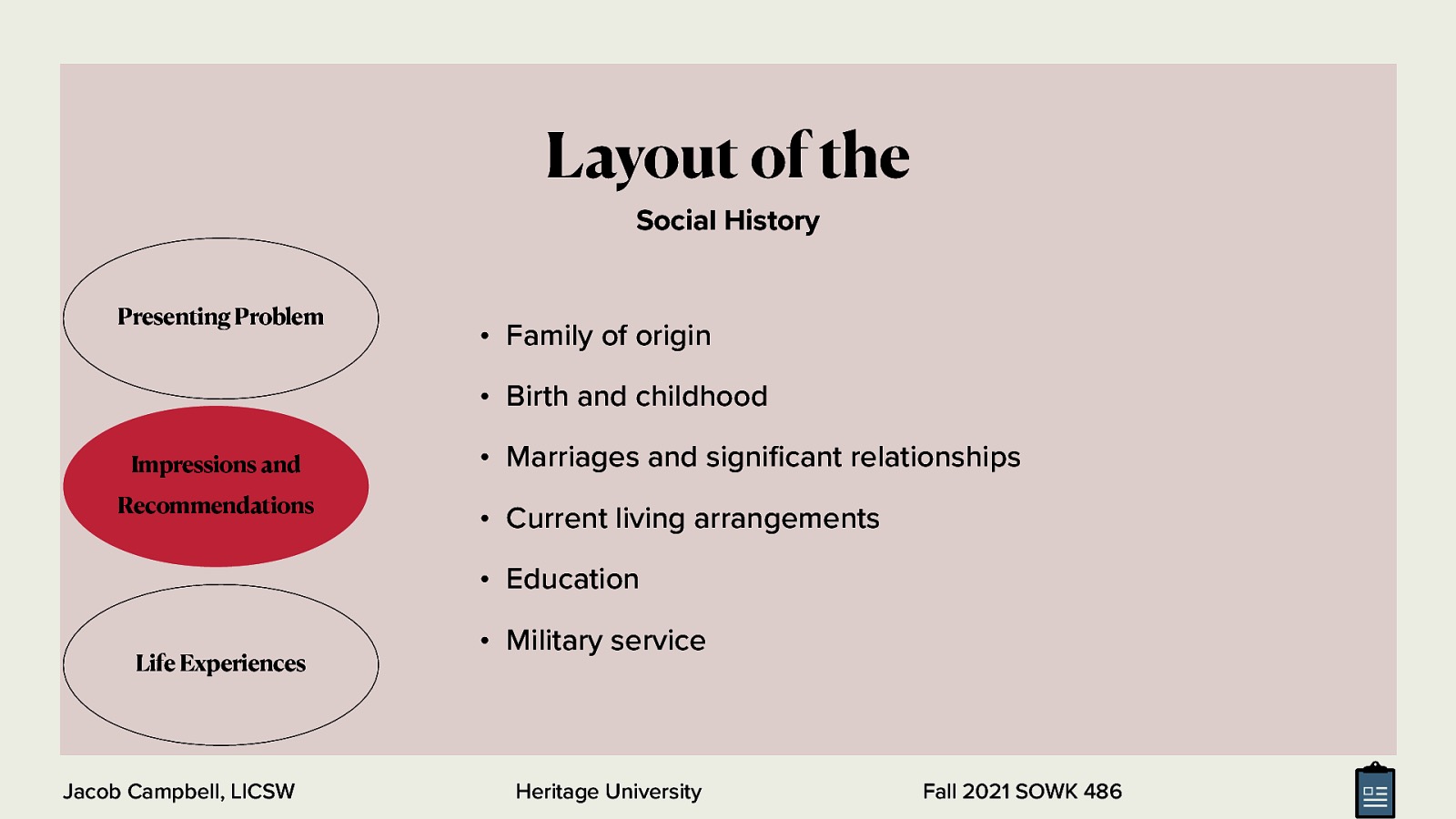
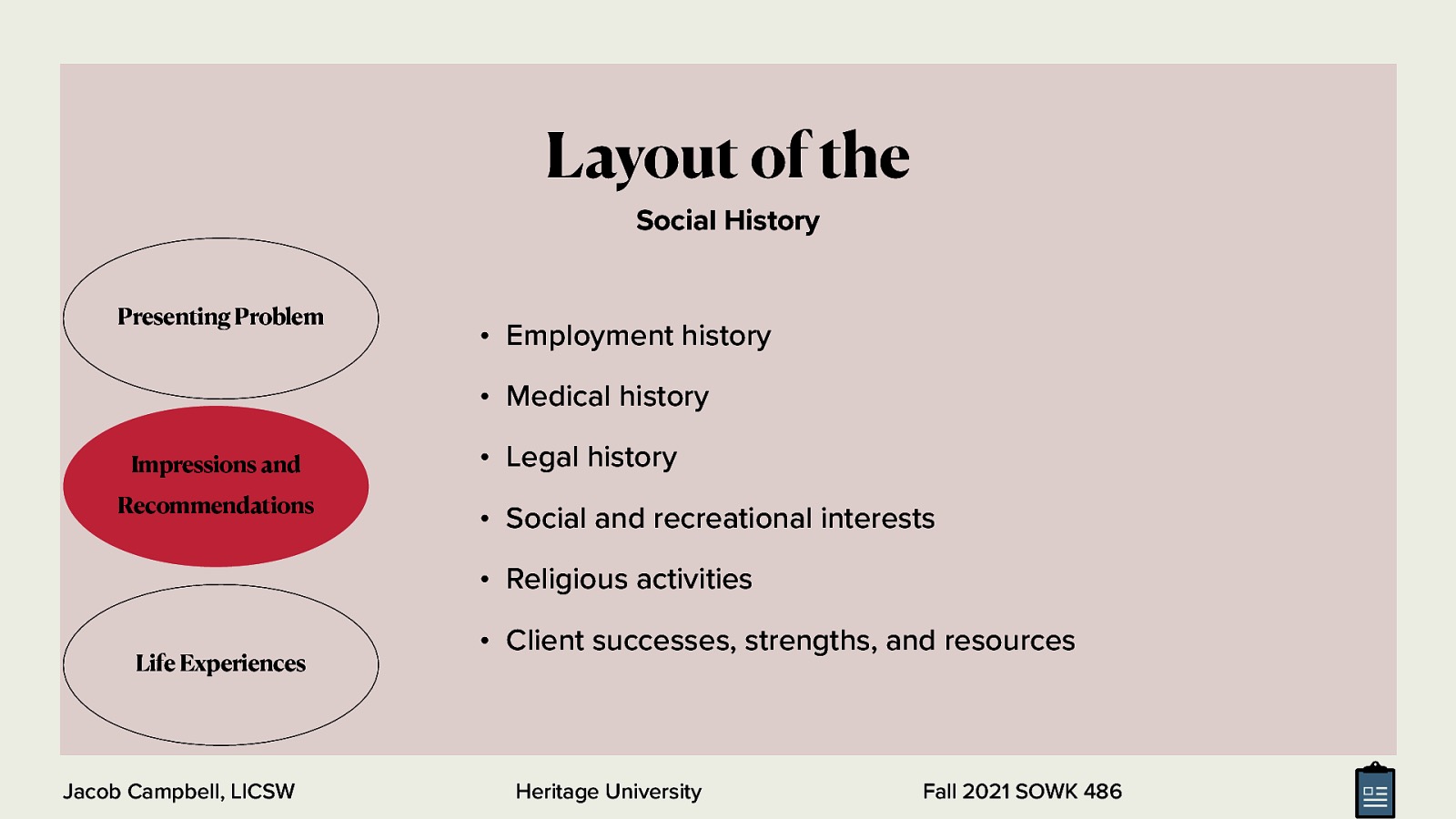
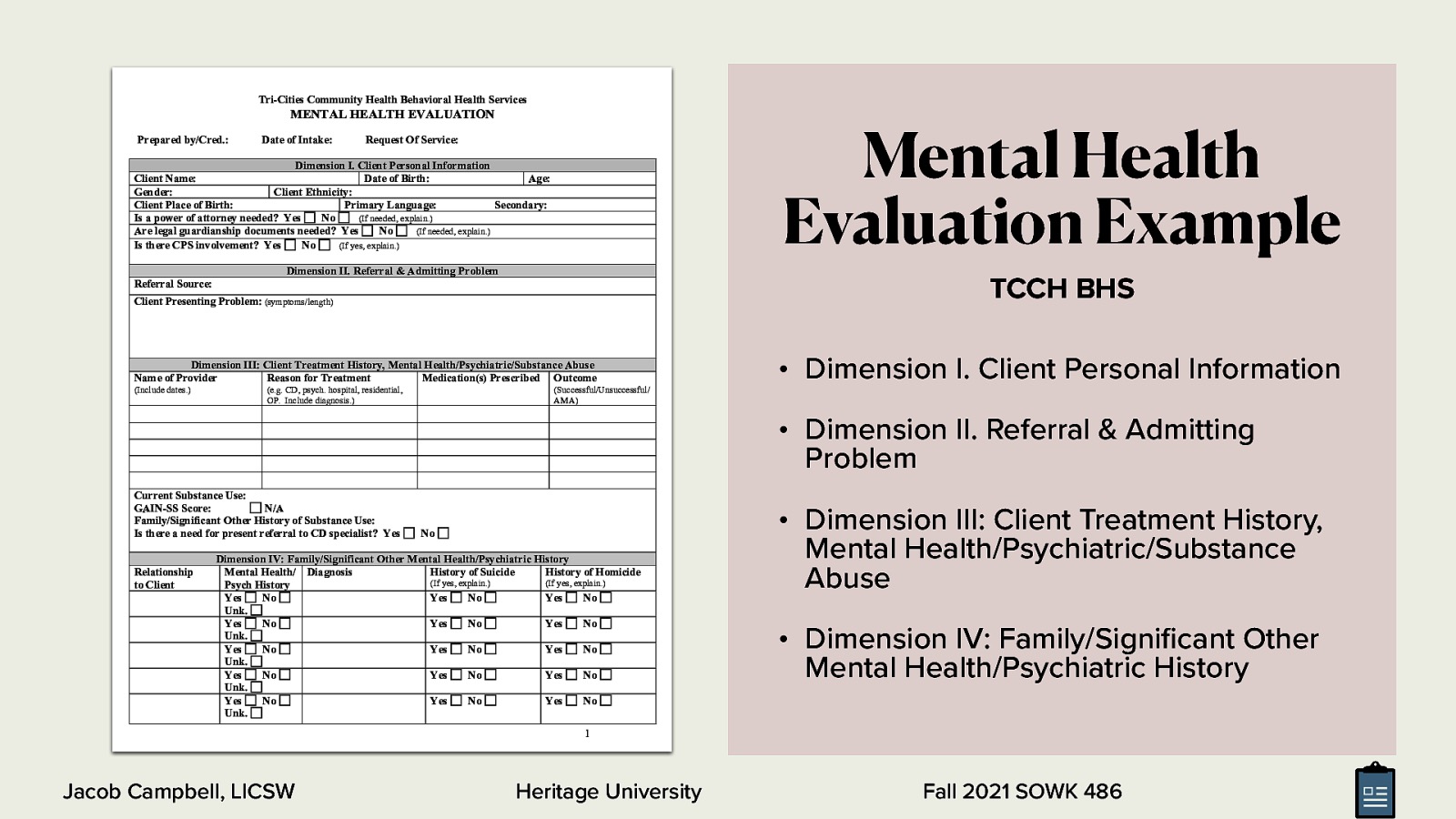
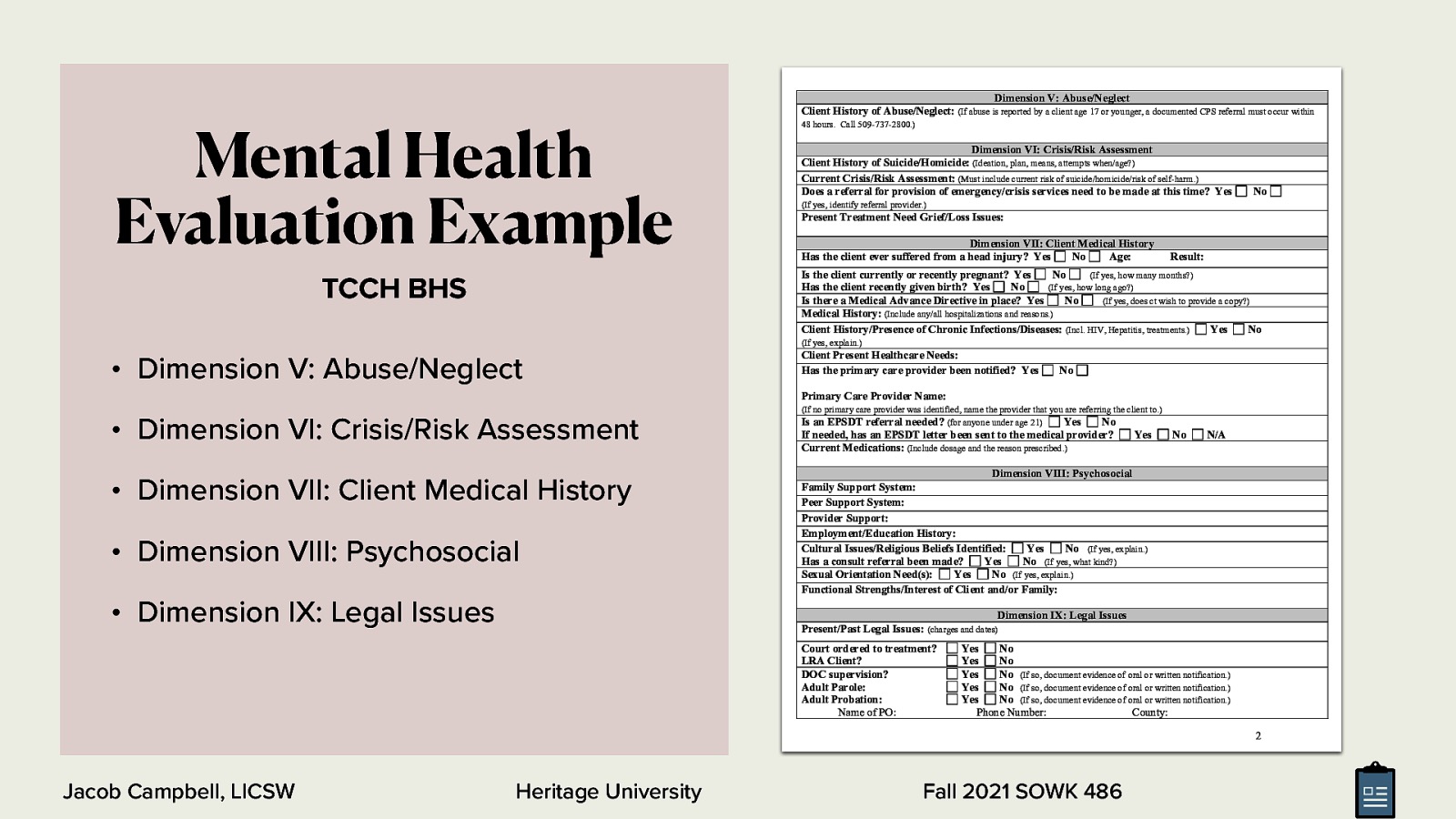
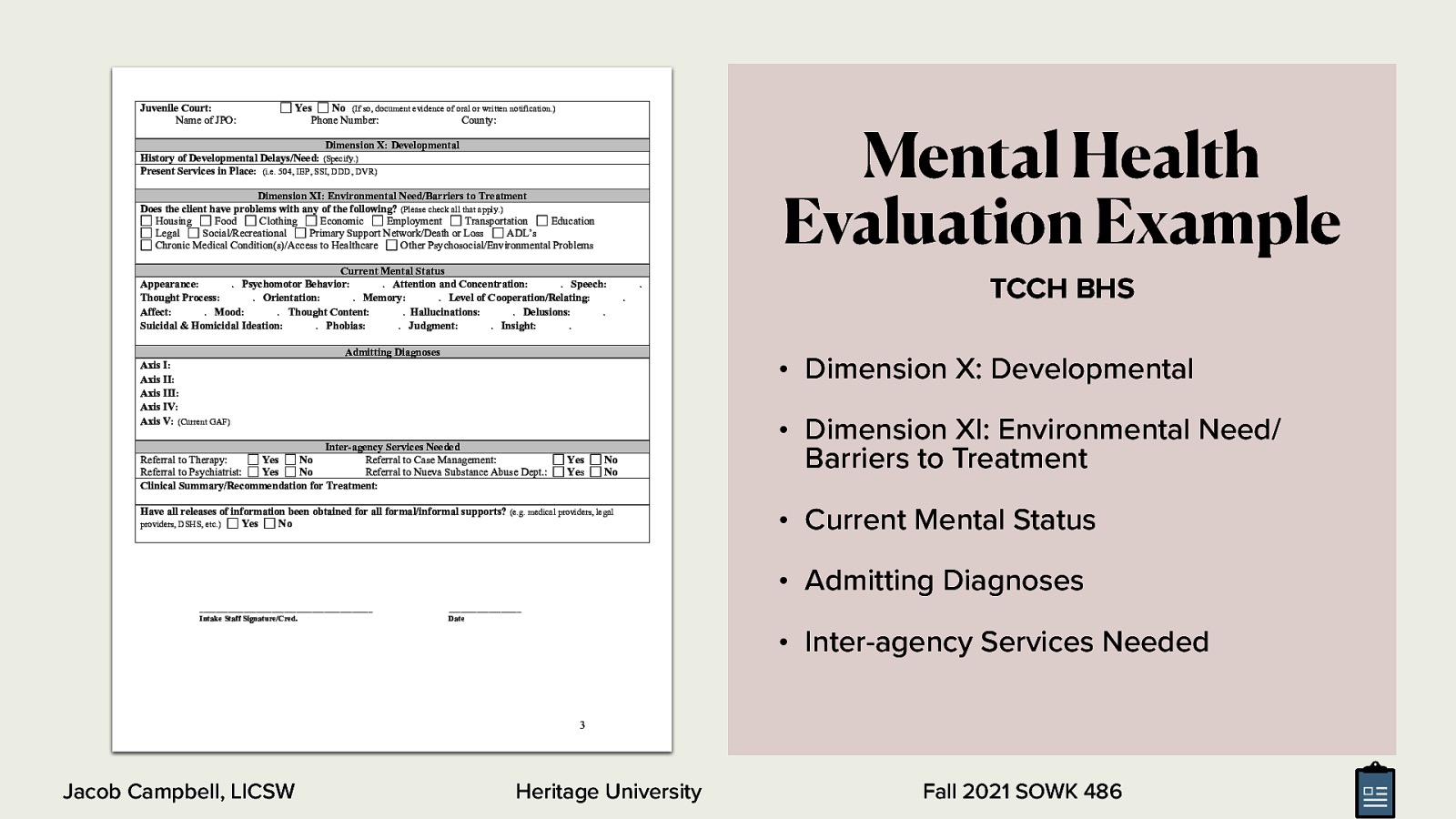
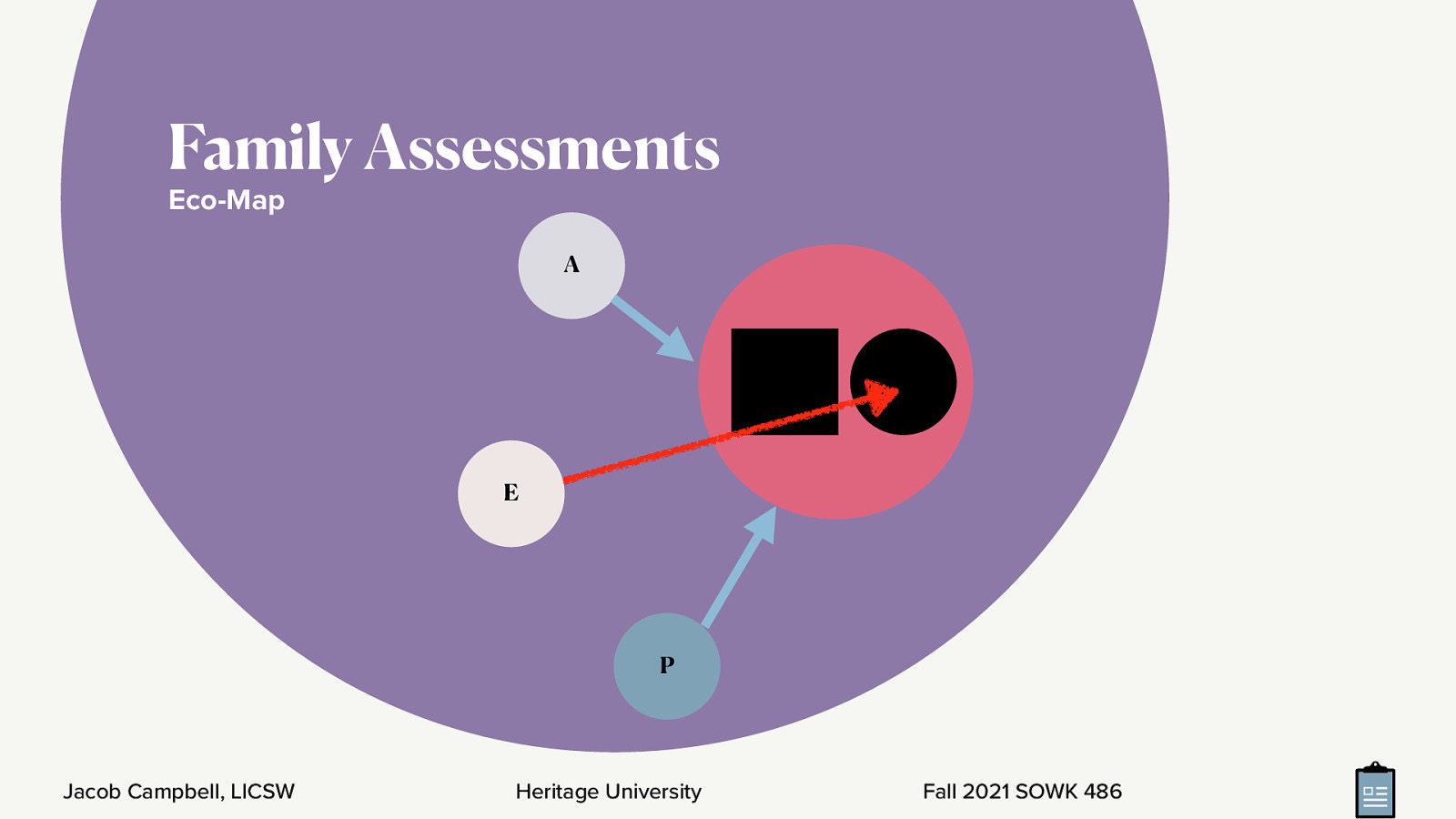
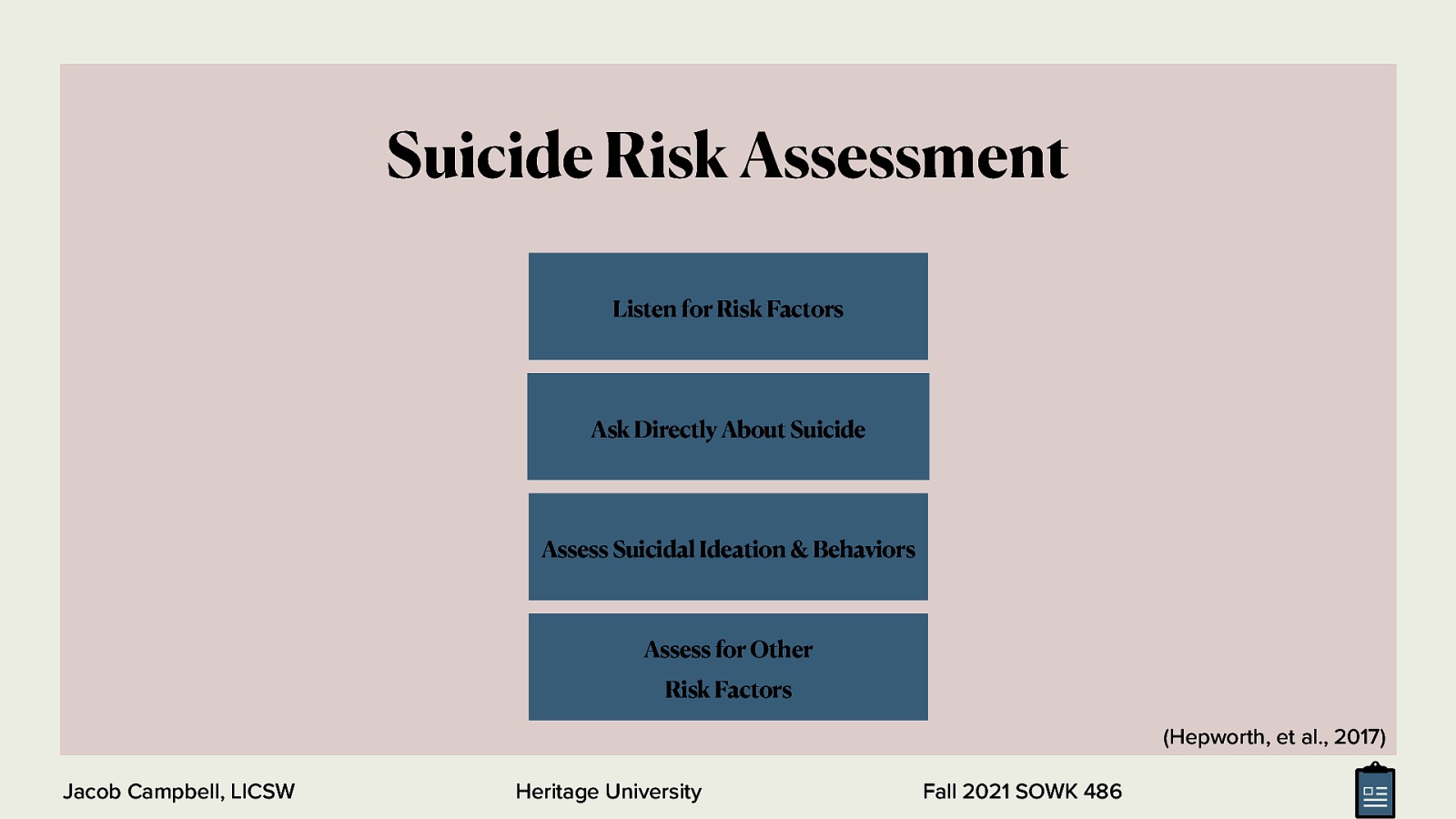
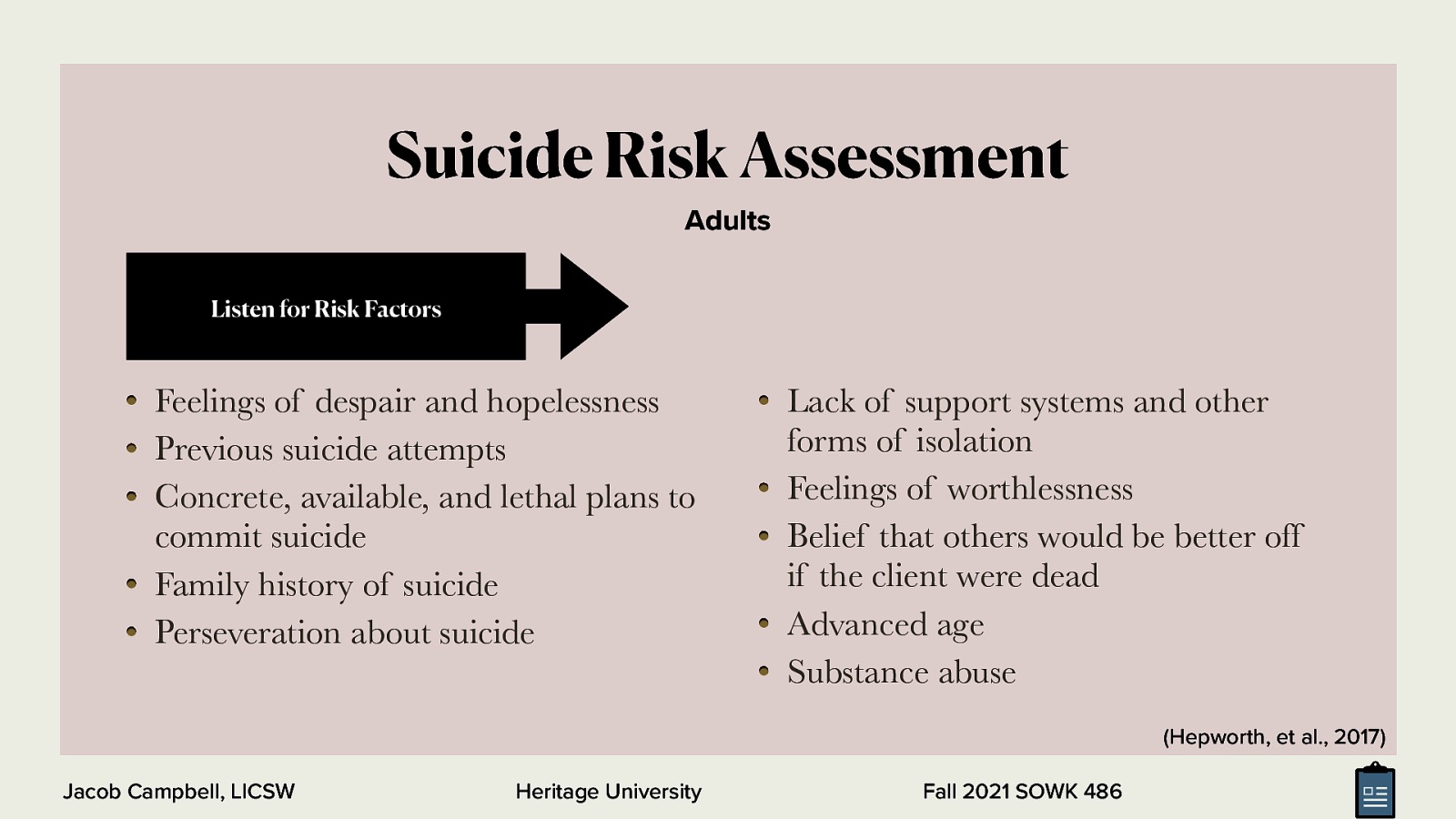
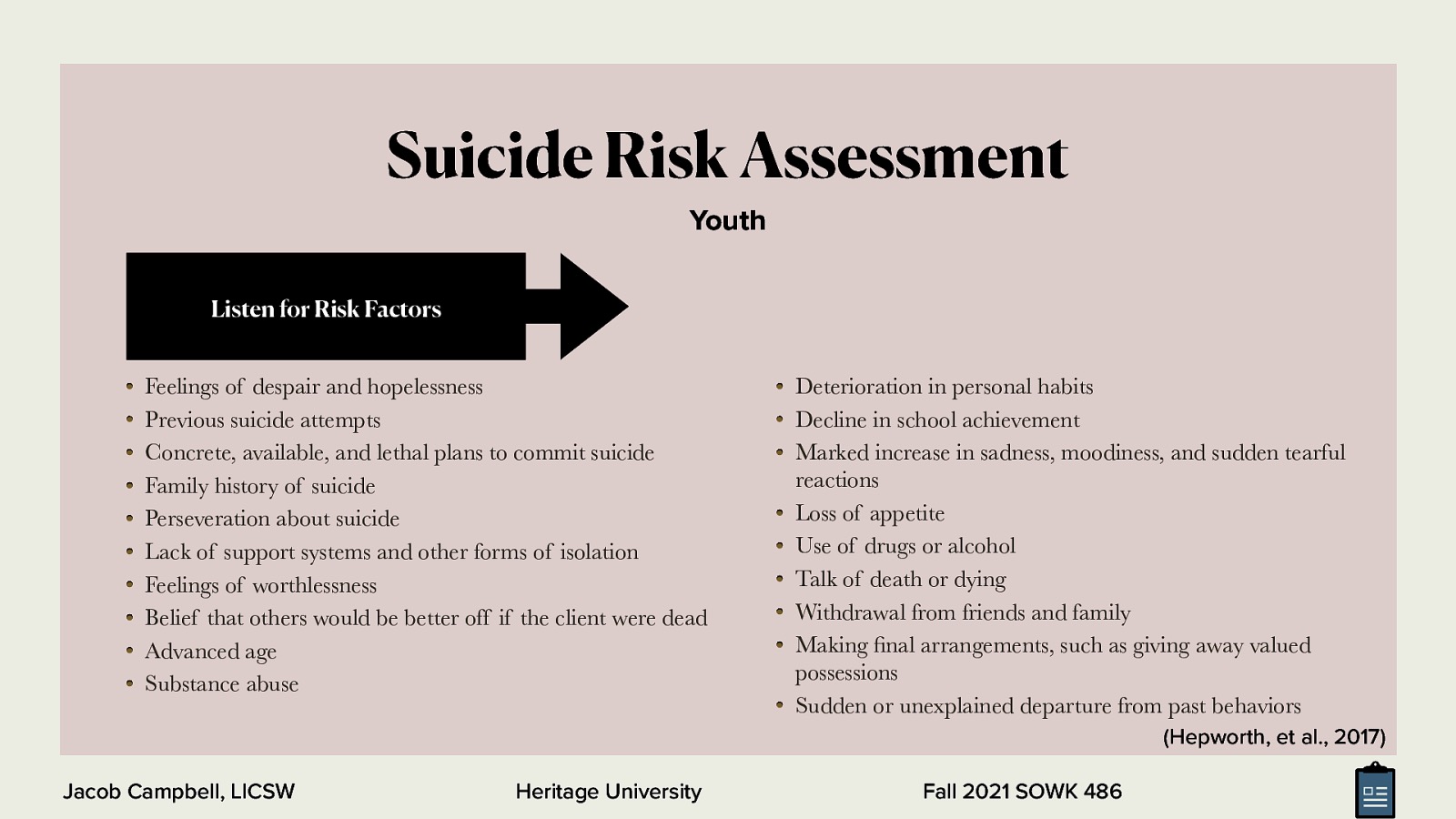
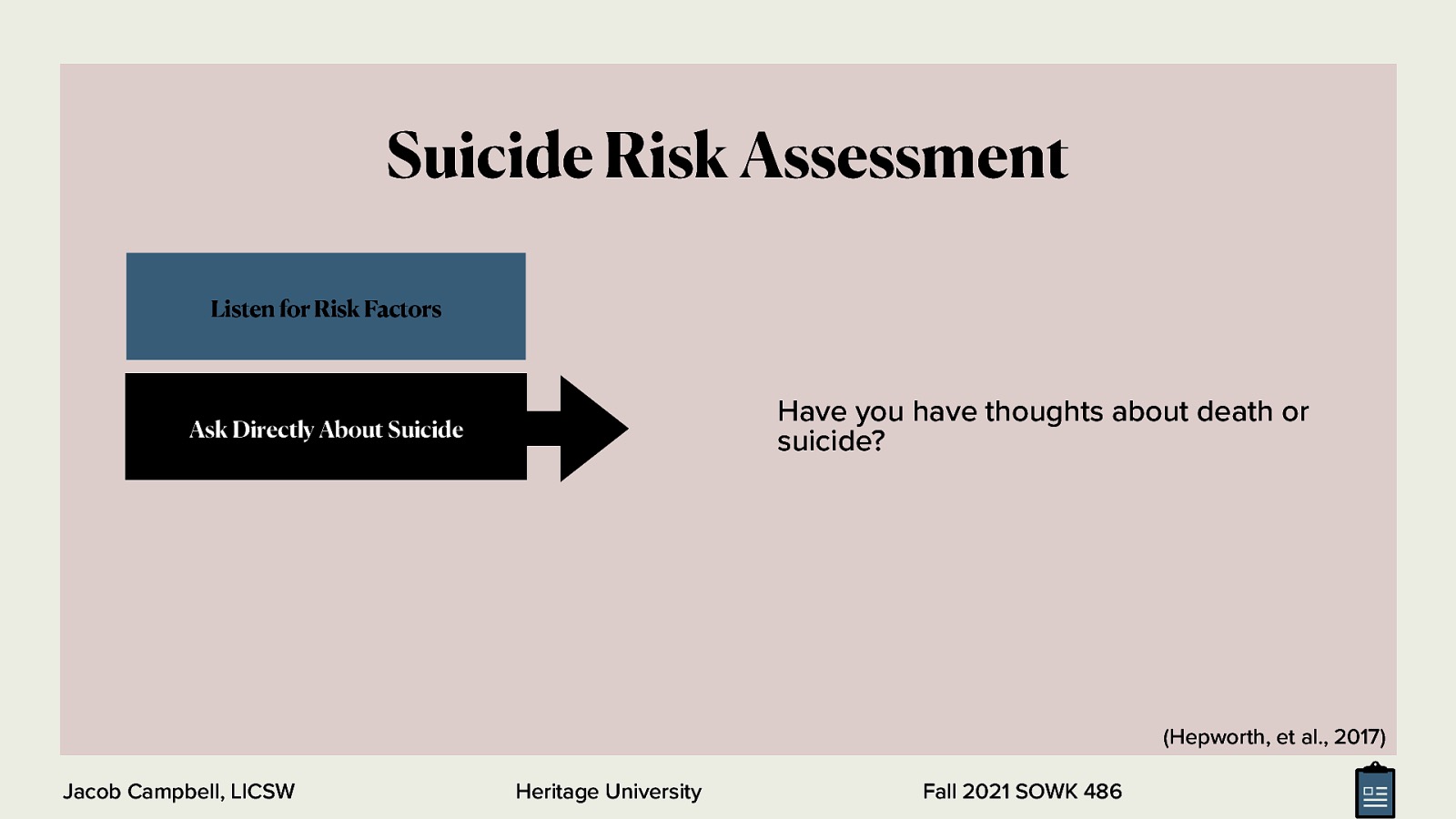
Week nine is a continuation of the work we started in week seven and looking at assessments. The focus is diving more into social histories, with an opportunity to practice asking questions related to this in small groups. As well, students do their teach-back activity if there is time we will do some activities around genograms and eco-maps.